Use Spinning Anxiety Ring in This Way for Quick Result

Anxiety is a growing concern for millions around the world, affecting people of all ages and backgrounds. From everyday stress to more serious conditions, the need for effective coping mechanisms is crucial. One innovative tool that has emerged to aid in stress and anxiety relief is the spinning anxiety ring. These rings, also known as fidget rings, have gained popularity for their calming effects. But how exactly can you use a spinning anxiety ring in a way that delivers quick results? In this article, we’ll explore how to harness the full potential of these rings and offer practical, research-backed advice on incorporating them into your daily routine.
What is a Spinning Anxiety Ring and How Does it Work?
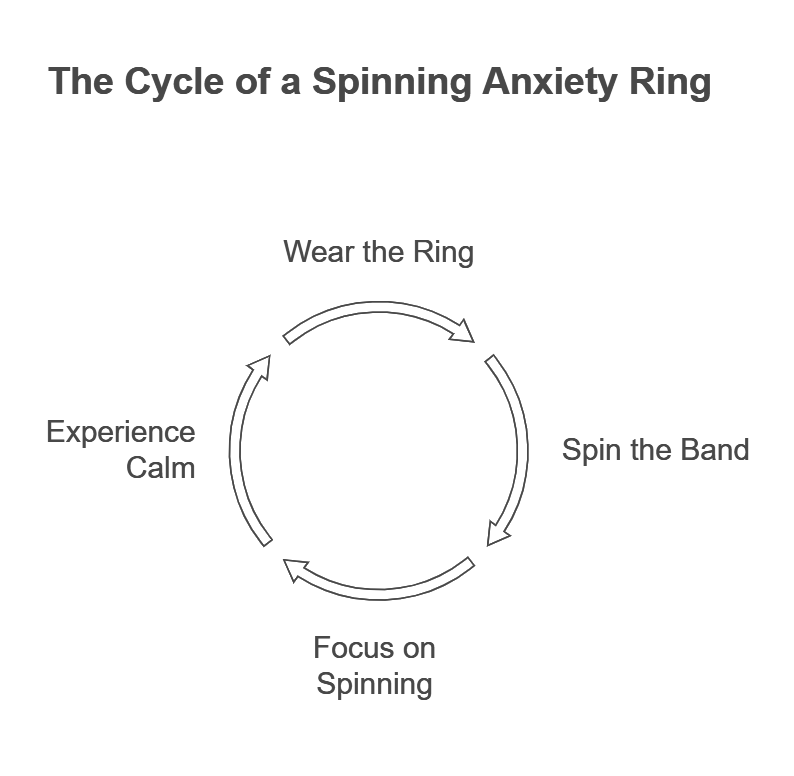
A spinning anxiety ring is a type of jewelry designed with a rotating component that allows users to fidget with it. Often crafted from metal, stainless steel, or titanium, these rings offer a soothing, tactile experience for those dealing with anxiety or stress. The action of spinning the ring helps to focus the mind, providing a form of mindfulness that can interrupt anxiety-inducing thoughts.
The key to understanding why these rings are effective lies in the concept of sensory stimulation. Fidgeting with a spinning ring engages the tactile senses, which can redirect focus away from anxiety-triggering thoughts. This is similar to other fidgeting tools, like stress balls or fidget spinners, which have been shown to reduce anxiety by offering a physical outlet for stress. According to a study by the American Psychological Association, physical distractions, like sensory toys, are effective in reducing physiological and psychological anxiety.
The Psychological Benefits of Spinning an Anxiety Ring
Using a spinning anxiety ring can significantly impact your mental well-being, particularly in moments when you feel overwhelmed by stress or anxiety. The benefits stem from two primary psychological mechanisms:
- Distraction: Spinning the ring provides a sensory distraction that helps your mind break away from spiraling, anxious thoughts. By focusing on the sensation of the spinning, your brain can shift its attention, preventing negative thought patterns from escalating.
- Grounding: The tactile nature of a spinning ring helps users stay grounded in the present moment. This type of grounding is an effective method in cognitive behavioral therapy (CBT), where patients learn to manage their emotions and reactions to stressors.
In fact, studies show that simple sensory grounding techniques, like spinning a ring or tapping your fingers, can activate the parasympathetic nervous system, which helps reduce stress and anxiety levels. As per a report from the National Institutes of Health, these techniques have been found to significantly lower cortisol levels. The hormone is directly associated with stress.
Use Your Spinning Anxiety Ring in This Way for Quick Results
To make the most out of your spinning anxiety ring, it’s important to use it correctly. Here are some expert tips and proven methods to ensure you achieve quick results:

1. Focus on Breathing While Spinning
The most effective way to use a spinning anxiety ring is by pairing it with deep, mindful breathing. The combination of focused breathing and the soothing motion of the ring can create a calming effect. This practice not only distracts you but also provides mental clarity, which is crucial in moments of heightened anxiety.
How to do it:
- Take a deep breath in for four counts.
- As you exhale, gently spin the ring on your finger.
- Focus on the tactile sensation and the feeling of the breath leaving your body.
According to a study published in the Journal of Anxiety Disorders, deep breathing exercises combined with mindful distraction, like spinning a ring, can lower anxiety levels almost immediately.
2. Use the Ring During High-Anxiety Moments
Spinning anxiety rings are most effective when used during moments of intense stress. Whether you’re at work, school, or in a social situation, having a spinning ring on hand can help you maintain calm in challenging environments. By using the ring in these situations, you can break the cycle of anxiety before it escalates.
Tip: Keep your spinning anxiety ring in your pocket or wear it at all times, so it’s accessible when you need it. You can also try wearing it on your dominant hand to make spinning easier and more natural.
3. Engage in Mindfulness While Spinning
One of the best ways to maximize the benefits of your spinning anxiety ring is by combining it with mindfulness techniques. This involves fully focusing on the experience of spinning the ring—its texture, movement, and the physical sensation it creates.
How to practice mindfulness with your ring:
- Close your eyes and focus solely on the feeling of the ring as you spin it.
- Notice the rhythm and the change in movement as the ring rotates.
- Let go of any anxious thoughts and simply observe the sensation.
This technique draws from mindfulness-based stress reduction (MBSR), a well-established method for managing anxiety. Research has shown that individuals practicing mindfulness in stressful situations experience a reduction in cortisol levels and a heightened sense of control over their stress.
4. Use the Ring for a Few Minutes Each Hour
To achieve quick results, consistency is key. By spinning your ring for just a few minutes each hour, you can keep your anxiety levels in check throughout the day. It’s a simple technique that doesn’t require a lot of time, but can have a profound effect on how you feel.
Pro Tip: Set a reminder on your phone to use the ring at regular intervals, such as every 60 minutes. This ensures you don’t forget to take a break and use the ring for stress relief.
How Quickly Can You Expect Results?
While the effects of a spinning anxiety ring can be felt almost immediately, long-term relief comes from regular use. Most users report feeling calmer within minutes of using the ring, thanks to its combination of sensory stimulation and grounding techniques.
However, for sustained benefits, it’s essential to incorporate the spinning ring into your routine. Just like any anxiety management tool, consistency is key. A study by the Mayo Clinic found that practices such as mindfulness and fidgeting can reduce anxiety symptoms when done regularly, resulting in longer-term improvements.
Scientific Studies Supporting the Use of Spinning Anxiety Rings
While personal anecdotes and testimonials are valuable, scientific research also supports the use of sensory tools like spinning anxiety rings. Studies show that small physical movements, including fidgeting, can reduce the brain’s response to stress and anxiety.
- A 2019 study from the University of California, Berkeley, found that engaging in physical fidgeting behaviors led to lower physiological markers of stress, such as heart rate and blood pressure.
- According to a 2016 report from the Journal of Clinical Psychology, using tactile objects to focus on the present moment is a powerful method for interrupting anxiety cycles, leading to quick relief.
Choosing the Right Spinning Anxiety Ring for You

Not all spinning anxiety rings are created equal, and choosing the right one can enhance your experience. Look for rings that are comfortable to wear, durable, and made from materials that feel pleasant to the touch. Some popular materials include:
- Stainless Steel: Durable, lightweight, and hypoallergenic.
- Titanium: Known for its strength and sleek design.
- Wood: Provides a natural feel and is often used in mindfulness-focused rings.
A 2017 survey from the Anxiety and Depression Association of America found that over 70% of individuals with anxiety preferred sensory tools that felt good on their skin, which is why material selection is so important.
Common Myths About Spinning Anxiety Rings
As with any tool, there are a few misconceptions about spinning anxiety rings. Let’s clear some of them up:
Myth 1: “The spinning ring can cure anxiety completely.”
Reality: While spinning a ring can be an effective tool for managing anxiety, it’s not a cure. It’s a helpful coping mechanism, but for long-term results, a combination of techniques such as therapy, medication, and lifestyle changes may be necessary.
Myth 2: “Spinning a ring will only help during moments of extreme anxiety.”
Reality: Spinning anxiety rings can help in mild to moderate anxiety as well. Regular use can prevent anxiety from building up to extreme levels.
Conclusion
Spinning anxiety rings are a simple yet powerful tool for managing anxiety and stress. By using them correctly paired with mindfulness, deep breathing, and regular use. You can experience quick relief from anxiety. With the right techniques, a spinning anxiety ring becomes more than just a trendy accessory; it becomes a reliable tool for everyday calm. If you’re looking for a way to ease your anxiety and regain control over your thoughts, give a spinning anxiety ring a try. It may just be the quick fix you need.